Synergy Spine and Pain Center
Pain Management Experts & Specialists to Help You Live Livelier!
Synergy Spine and Pain Center offers the best customized comprehensive pain management treatments to help you get back to daily life activities. Our doctors service patients from all over the DMV area with the best methods, treatments and care possible to let you Live Livelier!

Synergy Spine and Pain Centers
Interventional Pain Management Specialists
Our mission is to provide effective treatments for early relief & recovery from acute and chronic pain, thereby enabling people to live livelier!
- We treat dozens of pain conditions from head to toe.
- Our safe and advanced interventional pain management treatments provide alternatives to major surgeries.
- We strictly follow guidelines for safe opioid management.
- We provide quick and reliable appointments.
- We accept most major insurance plans and providers.
We Care About You
We Provide the Best Pain Management Solutions
Dr. Madhavi Chada and her team have provided over twenty five years of pain management services and patient relief to the DMV area.
Location 1
- Bowie / Glenn Dale, MD
12150 Annapolis Road, Suite 209
Glenn Dale, MD 20769
- (240) 929-6652
Location 2
- Fort Washington, MD
10709 Indian Head Hwy, MD-210, Suite D
Fort Washington, MD 20744
- (240) 260-3828
Location 3
- Silver Spring, MD
11233 Lockwood Drive
Silver Spring, MD 20901
- (240) 641-5922

Madhavi Chada, MD
Pain Management Physician
TOP Interventional Pain Management Physician
Dr. Madhavi Chada is recognized as a TOP Interventional Pain Management Doctor throughout the Maryland region and is featured on the TOP Doctors Interviews which are seen on CNN Headline News, FOX News, Oprah Winfrey Network, BRAVO, CNBC, MSNBC and other networks.

Madhavi Chada, MD
Pain Management Physician
TOP Interventional Pain Management Physician
Dr. Madhavi Chada is recognized as a TOP Interventional Pain Management Doctor throughout the Maryland region and is featured on the TOP Doctors Interviews which are seen on CNN Headline News, FOX News, Oprah Winfrey Network, BRAVO, CNBC, MSNBC and other networks.
Our Services
Our Team Can Help You
With a Variety of Services
Synergy Spine and Pain Center offers a plethora of pain management options to help decrease or relieve pain and increase your quality of life!

Epidural Injections
Delivery of powerful anti-inflammatory medicine directly into the spine to reduce pain and inflammation.
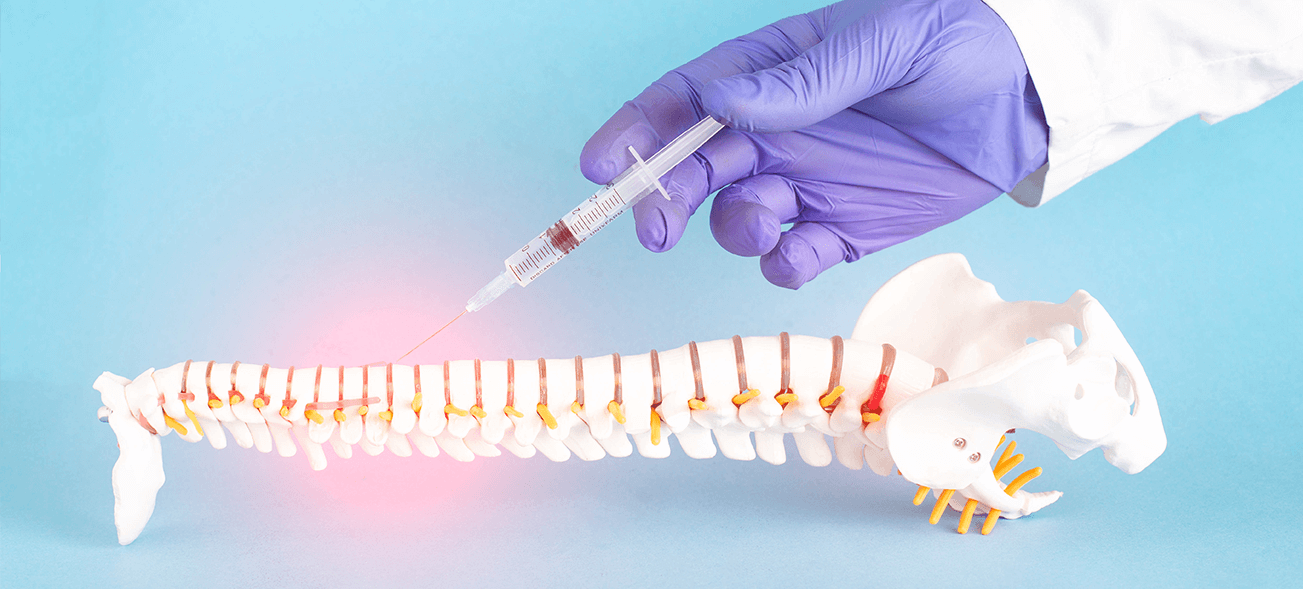
Selective Nerve Blocks
Long-lasting steroid (cortisone) injection around the nerve root to help reduce inflammation and pain.

Sacroiliac (SI) Joint
Low back pain treatment that helps decrease pain and inflammation from SI joint dislocations and issues

Rhizotomy
Killing nerve fibers in the affected area to reduce pain by preventing the body from sending pain signals to the brain.

Discography
Diagnostic procedure that helps determine which, if any, disc in your spine is the source of your pain

Kyphoplasty
Restores the original shape and positioning of an injured vertebra and relives pain from spinal compression
Why Choose Us
Simple, Supportive Healthcare
Friendly Staff
We pride ourselves in how we work with our patients and our ability to enhance their lives.
Successfulness
All of our patients receive some form of relief for their pain, whether it is by reduction or completely curing the cause.
Reliability
We are available at multiple locations and provide the best care to our patients in a reasonable time frame.

Testimonials
What Our Patients Say About Us
Our patients love our pain management options and they let us know how much we have helped them manage their conditions!
Contact us
If you Have Any Questions Schedule an Appointment
Contact Synergy Spine and Pain Center today
to relieve your pain and live livelier!
